People who have not been vaccinated against Covid-19 are still repositories of novel variants of SARS-CoV-2 worldwide. But this also applies to immunosuppressed people who cannot cope with such an infection. This is evidenced by a case report of a person living with HIV in South Africa, which has now been presented at the annual conference of the European Society for Clinical Microbiology and Infection (ECMID/Online).
“The new mutations (from SARS-CoV-2; note) allow pathogens to evade the immune system. This means that antibodies formed as a result of a previous natural infection or vaccination no longer do well before they protect against other infections,” said Alex Segal, who works At the Max Planck Institute for Infection Biology in Berlin and at the African Institute for Health Research (KwaZulu-Natal/South Africa).
It’s time to transform
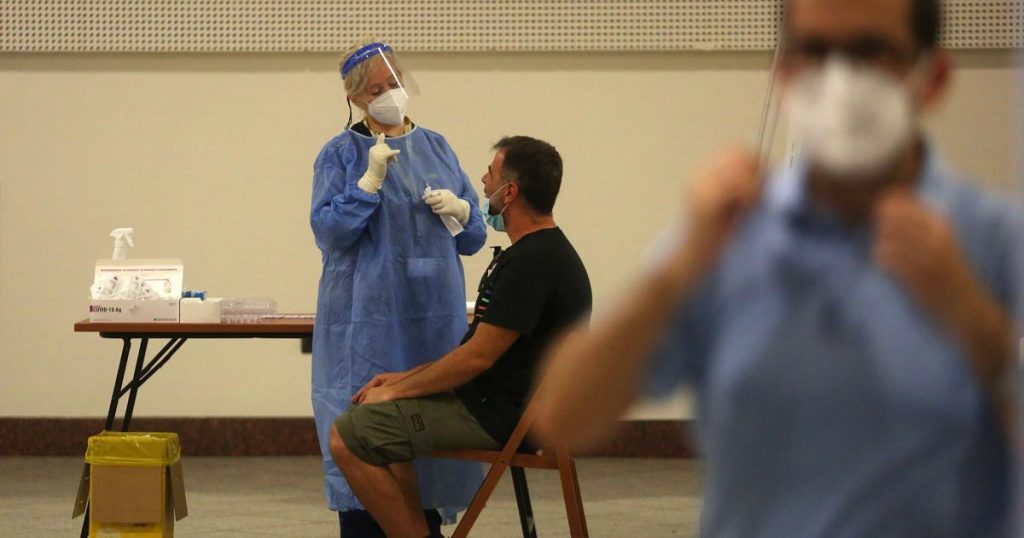
In South Africa, SARS-CoV-2 encountered HIV in the recent past. According to the scientist, there is increasing evidence that the South African variant (Beta-SARS-CoV-2) of Covid-19 leads to severe disease cycles in people with HIV infection on the one hand, and more dangerous mutations on the other hand. Segal presented the case of a South African AIDS patient with uncontrolled HIV. “Although she had a mild illness from COVID-19, her SARS-CoV-2 tests remained positive for 216 days,” broadcast to the Conference of European Microbiologists and Infectious Agents said.
“While most people overcome SARS-CoV-2 quickly, there are indeed some reports of long-term infection in immunosuppressed people,” the team of authors wrote in their study, which has not yet been published in a peer-reviewed scientific journal.
The patient described was a South African woman who was just under 40 years old and came to the hospital twelve days after developing a sore throat and shortness of breath due to SARS infection. The woman had been HIV positive since 2006 and was on antiretroviral therapy, she also had asthma and was treated with a cortisone spray and a bronchodilator. It seems that anti-HIV treatment was not enough. Changing the hospital medication led to detection of HI viruses below the detection limit only after 206 days.
The pathogen evades
However, during this time, the patient remained positive for SARS-CoV-2. Only after day 216, the pathogens of Covid 19 are no longer detectable. The core turned out to be the multiple sequences of the pathogens of Covid-19: the E484-K substitution mutation of SARS-CoV-2, an “escape variant” of the pathogen, developed relatively early in women. As a result, other types of SARS-CoV-2 were detected in the woman. “This is an indication that the evolution of viruses in vectors of the pathogen represents a mechanism for the development of SARS-CoV-2 mutations, which can evade the immune response,” the experts wrote.
Individual and group vaccination
The necessary consequences are obvious: in the case of immunosuppressed people, special attention should be paid to vaccination prevention and also to an adequate immune response after full vaccination. This would be necessary for cancer patients and other patients around the world who are on immunosuppressive therapy for their primary disease, for example.
However, according to the World Health Organization (WHO), there are about 37.9 million people living with HIV worldwide, and more than 20 percent of them are unaware of their infection. All should be given antiretroviral treatment for HIV so that their immune system is able to quickly overcome any infection with the Coronavirus. Of course, it will be critical to achieve adequate vaccination protection worldwide to fend off an epidemic.

“Total coffee aficionado. Travel buff. Music ninja. Bacon nerd. Beeraholic.”





More Stories
Study: Working full-time can affect your risk of cancer
The new “Karl” has arrived – Focus: Psychology
Psychology: 3 strategies to help when you can't concentrate